Dental Arts of Oklahoma - Blog Page
Tips, Facts, And The
Latest In Dentistry

What To Know About Complications From Dental Implants
Posted in Dental Implants
Dental implants are a durable way to replace missing teeth. They look and act like natural teeth and are used more often now than ever. Still, no surgery is risk-free. Understanding complications from dental implants and the warning signs can help you get care early and protect your smile.
What Causes Complications From Dental Implants?
– Infection: Bacteria at the implant site can cause early or late problems, stopping healing and damaging bone. – Poor planning: Inaccurate implant placement can hit nerves, sinuses, or leave weak bone support. – Inadequate bone: If the jaw lacks bone, implants can fail unless grafting is done first. – Surgical trauma: Excessive force or heat during drilling can harm bone and tissue. – Patient health issues: Conditions like uncontrolled diabetes or habits like smoking slow healing and raise risk. Each cause affects healing or the long-term stability of the implant. Knowing these helps you and your dentist plan safer treatment.
Common Early Complications
Infection and implant site inflammation
Infections often show up within days to weeks after surgery. Look for redness, swelling, increased pain, warmth, a bad taste or smell, and possibly fever. Early treatment with cleaning, antibiotics, and improved hygiene usually controls infection and preserves the implant.
Bleeding and wound problems
Some bleeding after surgery is normal, but heavy or prolonged bleeding is not. If blood soaks through dressings, or you develop large clots or open wounds that won’t close, call your dentist. Persistent bleeding can delay healing and raise infection risk.
Nerve injury and altered sensation
Nerve issues can cause numbness, tingling, burning, or sharp pain in the lip, chin, tongue, or gums. These symptoms may start right after surgery. Some nerve injuries are temporary; others need urgent evaluation to prevent long-term loss of feeling.
Common Late Complications
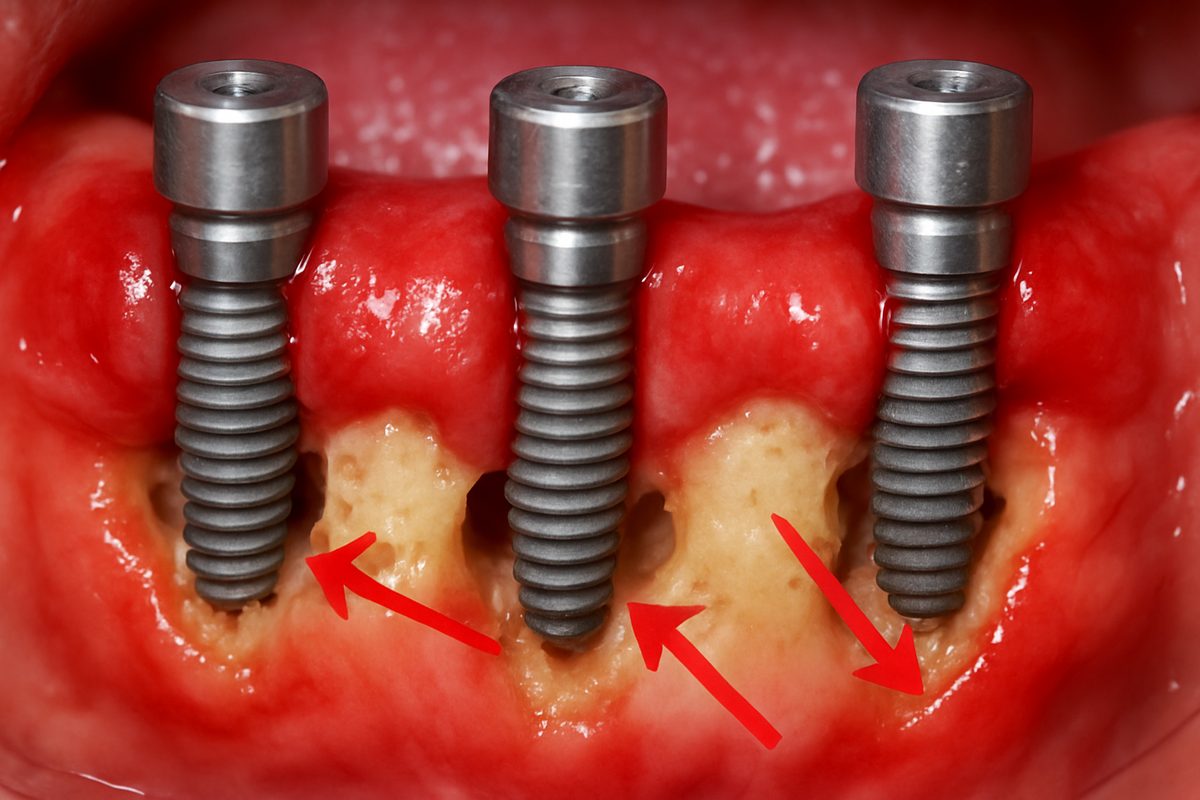
Peri-implantitis (bone loss and gum disease around implants)
Peri-implantitis is like gum disease around a natural tooth but affects the implant and surrounding bone. Signs include bleeding gums, pus, bad breath, receding gum tissue, and loosening implants. Poor oral hygiene or past gum disease increases the chance it will occur.
Implant loosening and prosthetic failures
Implants can loosen because of bone loss, poor fit, or overwhelming biting forces. Prosthetic parts (crowns, screws, bridges) may fracture, loosen, or wear. Many prosthetic problems can be fixed, but repeated failures may require implant revision or removal.
Who Is At Higher Risk?
Higher risk groups include smokers, people with uncontrolled diabetes, those with poor oral hygiene, and patients with a history of gum disease. Anatomic risks include thin bone, close proximity to the sinus, or existing nerve paths. Certain medications, chemotherapy, or radiation to the head and neck also raise complication risks.
How Dentists Diagnose Complications
Dentists use a clinical exam to check for redness, swelling, mobility, and signs of infection. Digital X-rays and CBCT scans show bone levels, implant position, and nerve proximity. Intraoral cameras help document soft-tissue health and teach patients how to improve care. Together these tools let clinicians detect problems early and plan treatment.
How Complications From Dental Implants Are Treated
Non-surgical care
Early problems often respond to improved oral hygiene, professional cleanings, antimicrobial rinses, and antibiotics. Pain control and short-term adjustments to chewing can help healing. Non-surgical care is the first step for mild infections and inflammation.
Surgical solutions
If non-surgical steps fail, surgery may be needed. Treatments include cleaning infected tissue (debridement), bone grafting to rebuild lost bone, soft-tissue grafts to cover exposed implant parts, or removing a failing implant. Reimplantation may be possible after healing and proper planning.
Prosthetic fixes
Many late issues are mechanical. Dentists can tighten or replace screws, remake crowns or bridges, and adjust bite forces. Proper prosthetic care often prevents further damage and restores function without surgery.
How To Reduce Your Risk Before Getting Implants
Prepare well: share a full medical history, stop smoking, and get blood sugar under control if you have diabetes. Complete dental cleaning and treat any gum disease first. Advanced imaging (CBCT) and guided surgical planning reduce surprises. Choosing an experienced implant team lowers the chance of complications.
When To Seek Care — Warning Signs Not To Ignore
Call your dental provider right away for spreading swelling, fever, severe pain that won’t ease, new or worsening numbness, visible implant mobility, persistent bleeding, or any pus draining from the site. Early action often prevents more serious outcomes.
Choosing a Provider Who Minimizes Complications
Providers who use CBCT, guided planning, and have dedicated implant experience tend to have better results. For example, Dental Arts of Oklahoma and Dr. Soren Michaelsen use CBCT imaging, All-on-4 planning, and full-scope implant care to reduce risks and improve predictability. Ask about technology, training, and follow-up care when choosing a team. You can read some of our patient stories here to understand our commitment to excellence, or learn more about us.
Conclusion and Next Steps
Most complications from dental implants are preventable or treatable when found early. Good planning, careful surgery, and solid home care cut your risk. If you are planning implants or have signs of trouble, schedule a consultation so a trained implant team can evaluate you and recommend the safest path forward.




